Constant readers, huge news: SUPERBUG will be featured in a segment today on the NPR program Fresh Air with Terry Gross. Please tune in if you can! Fresh Air‘s broadcast times vary across the country, but you can listen online or via podcast. The schedule is here.
One week to publication! And the book video is up
OK, folks, mystery unveiled: Here’s what I look and sound like. Simon and Schuster has put up a video for the book — not a trailer, per se, but an interview with me (backed by spooky music!).
I’m having trouble with the embed code – I can’t seem to resize their monster window! — but meanwhile the link is here.
UPDATE: How’s this?
Get Smart About Antibiotics Week, Oct. 5-11 (now!)


Every year, the CDC sponsors a week-long observance called Get Smart About Antibiotics Week, intended to bring attention to this issue of antibiotic misuse that all of us here are so concerned about, and to link the efforts of federal and state agencies, nonprofit groups, and anyone else with an interest.
Today marks the start of the 2009 week, and of course it comes as a crucial time: With the H1N1 flu pandemic causing so many people to seek care for upper respiratory illnesses, the possibility of antibiotics being misprescribed for a viral illness is greater than usual.
The homepage for the CDC campaign is here. There is an abundant list of materials, images, campaign strategies and suggestions for framing the conversation, along with graphics (I’ve lifted the one at left from a poster aimed at parents of young children), PSA sound files, and cute little web widgets such as the image at right above (sorry for the poor layout skills, it’s a busy morning).
Since this comes from the CDC and is therefore taxpayer-funded, all of it is open-access. So go, already.
A reminder: It’s World MRSA Day
Decolonization: disappointing news
I know that many of you who are MRSA patients, especially with recurrent infections, are especially interested in the issue of decolonization, the grueling regimen of antibiotic nasal gel (containing mupirocin; usually sold as Bactroban) combined with body washes with chlorhexidine (Hibiclens) that is believed to eradicate MRSA carriage in the nose and on the skin. Decolonization is an essential part of the “search and destroy” measures practiced by zero-tolerance hospitals who want to detect any MRSA transport in their institution, and it is a last-ditch hope in recurrent community-strain infections. (I told the story of several women’s struggles with recurrent infections in SELF and Health magazines.)
It’s disheartening, then, to realize that decolonization is not a universally agreed-upon measure, and there is relatively little research that can say in which setting (household, hospital, ICU) it works best, and why. There have been a few studies, and a few review papers summing up studies, on the role that decolonization can play in reducing the risk of infection in already hospitalized, colonized patients — ones about to undergo surgery, for instance. A meta-analysis by the Cochrane group, of 8 trials, found that decolonization in the hospital did reduce the likelihood of infections in surgical patients.
The role that decolonization can play in short-circuiting community infections is much less clear, though there are many, many people who have suffered recurrent infections and testify that it worked for them. (Please speak up in the comments if you are!) One problem is that outside hospitals, there is no one recommended regimen: One physician might tell her patient to use mupirocin and chlorhexdine only, whereas another might tell his patient to also take bleach baths, or bleach all the laundry or household surfaces. The CDC has so far declined to put its muscle behind decolonization in community-strain infections, recommending only that frustrated patients with recurrences seek the advice of an infectious-disease specialist. (See this flowchart of treatment options (.pdf) that the CDC published in 2007.)
Comes now the infectious-diseases division of Evanston Northwestern Healthcare, whom some of you will recognize as being among the most successful and evangelical practitioners of “search and destroy” in the United States. (ENW has recently been renamed NorthShore University HealthSystem and is affiliated with Northwestern University. Disclosure, in case you care: I went to grad school at Northwestern, though not in medicine.) In a paper published in Infection Control and Hospital Epidemiology, the group evaluates the use and success rate of decolonization in ENW/NorthShore’s 3 hospitals and finds, well, not such good news: a temporary reduction in patients’ being colonized with MRSA, but no success in preventing infection.
This is an important and troubling finding, because decolonization comes with costs. There is the obvious cost to hospitals (and the follow-on cost to insurance companies and consumers) of paying for mupirocin and chlorhexidine themselves. But there is also a hidden cost that we here should be particularly sensitive to: Because mupirocin is being used so lavishly, mupirocin resistance is rising.
In the same issue of ICHE (which, yes, is pronounced Itchy), a related editorial by Dutch researchers reviews the difficulty of conducting decolonization trials, but summarizes the ENW/NorthShore study as not an endorsement of decolonization regimens:
It is clear that staphylococcal carriage is an important risk factor for infection and that eradication of carriage has proven successful for patients who are undergoing elective surgery. For other groups of patients, it is still unclear what the benefits are. It is obvious that indiscriminate use of mupirocin is associated with development of resistance. Therefore, additional studies are warranted to define the optimal MRSA decolonization strategy, including what should be given, to whom, and at what moment and who should guide and supervise the regimen.
The cites are:
Robicsek A, Beaumont JL, Thomson RB Jr et al. Topical therapy for methicillin-resistant Staphylococcus aureus colonization: impact on infection risk. Infect Control Hosp Epidemiol. 2009 Jul;30(7):623-32.
Kluytmans J, Harbarth S. Methicillin-resistant Staphylococcus aureus decolonization: “Yes, we can,” but will it help? Infect Control Hosp Epidemiol. 2009 Jul;30(7):633-5.
Bad news from California
Constant readers, some of you may be aware that one major nexus of MRSA infection gets very little attention, though I’ve tried to raise it here periodically. That’s MRSA in jails and prisons: Thanks to poor hygiene and extraordinary overcrowding, jails and prisons are hotbeds of the bug, and it is very common for people to develop an infection after they are incarcerated, and then to be unable to shake it because they cannot keep up with hygiene, cannot get access to a doctor, etc.
Some commenters, here and elsewhere online, have suggested that this is no more than prisoners deserve. This seems to me both extraordinarily uncompassionate and epidemiologically foolish. In case no one has noticed, prison overcrowding is so serious that many prisoners don’t stay in prison for their sentenced time. And when they come out, and come back to their communities, they bring MRSA with them. That’s not even to mention the risk to the very large numbers of people who are not themselves incarcerated, but go in and out of jails and prisons every day: correctional officers, cooks, medical staff, and on and on.
All of which makes the news from California on Friday more than usually depressing.
Prison medical care in California has been so bad (see Gov. Arnold Schwarzenegger’s 2006 emergency declaration) that it is no longer under control of the state, but rather administered by a court-appointed receiver, who said in 2007:
Across the board we see delays in diagnosis and access to care and needed tests; misfiled, incomplete or illegible medical records; lack of space, sanitation and staffing; botched hand-offs of medical information during inmate transfers; failures by clinicians to recognize and evaluate “red flag” symptoms, follow published guidelines, perform basic physical examinations or respond to patient complaints; abdication of responsibility for patient care and lack of critical thinking or requests for help in difficult cases.
The prevalence of MRSA in California prisons is an important part of that picture : Correctional officers have sued over MRSA they acquired at work. (And yes, you can read all about it in SUPERBUG.)
Now, you may also know that California is in the midst of a gruesome budget crunch — and on Friday, the push for better prison medical care and the deficit in the state budget collided, and the deficit won. According to the Associated Press and the San Francisco Chronicle, the Schwarzenegger administration backed off an agreed-upon plan that would have ended the receivership and returned control of the medical system to the state at a cost of $1.9 billion, one-fourth of what was originally thought to be needed.
Schwarzenegger said in a statement Thursday that California cannot afford the additional cost.
“We cannot agree to spend $2 billion on state-of-the-art medical facilities for prisoners while we are cutting billions of dollars from schools and health care programs for children and seniors,” he said.
Schwarzenegger and lawmakers are considering eliminating or significantly reducing education, state parks and core social programs to address the $24.3 billion budget shortfall. (AP, byline Don Thompson)
The Chronicle story makes clear that the prison spending would not have made the deficit any worse, because the money was coming from new bonds, not from the state’s general fund. Its online commenters don’t seem to have paid attention to that, as they hit the same familiar themes:
- “Why should the public have to babysit them for the medical problems they brought on themselves… Let them rot.”
- “In my opinion bad medical services in prison should be only one of the deterrents that keeps one from wanting to go to jail. “
- “Prison should be a place that is so intolerable, that no sane person would ever want to go there.“
It’s easy to moralize. It’s much harder, as we know here, to control the continuing spread of a microbe that has already gotten a solid foothold in the community. California’s decision to not improve medical care in its prisons — and therefore not address the threat of MRSA to its prisoners and staff — is practically a guarantee that the state’s already substantial community MRSA problem is going to get much worse.
200th post! with thanks
Constant readers: Funny how one loses track. According to the dashboard, this is my 200th post at SUPERBUG. I’m thrilled and humbled that we’ve been able to build this solid community in support of more attention to this very under-appreciated disease. You are the ones that make it happen, and I am very grateful.
Kindle owners: My first book now available, with a MRSA chapter
It was news to me, until a friend of mine went and bought it: My first book, Beating Back the Devil: On the Front Lines with the Disease Detectives of the Epidemic Intelligence Service, has been put into a Kindle edition.
BBtD was the first and so far only book to go inside the CDC’s “outbreak police.” It tells a year in the life of the first class of young physicians and PhDs to join the Epidemic Intelligence Service after the anthrax attacks — the first year, in other words, in which the EIS officers knew in advance that the possibility of confronting bioterrorism was no longer hypothetical. It tracks members of the class around the planet, from West Nile virus to foodborne illness to malaria prevention in Malawi to SARS. In alternating chapters, it also tells the hidden history of the EIS, which was founded in 1951 as a post-Korean War force for bioterror detection. Its members were in on every major disease event of the second half of the 20th century: the launch and near-failure of the polio vaccine, the end of smallpox, the beginning of AIDS, and the emergency investigation of the anthrax attacks (during which I was embedded with a CDC team).
Most important for our purposes here, BBtD takes you inside an investigation of a MRSA outbreak — in Los Angeles in 2003, when gay men who frequented sex clubs began developing cripplingly serious skin infections, and a young CDC investigator had to determine whether to call on the city to shut the clubs down…
A little public-health humor
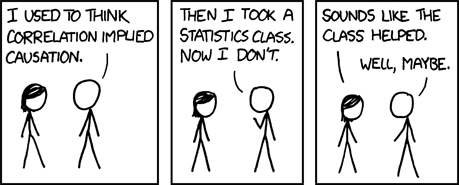
Constant readers – lots of new news happening, and blogposts coming. While I organize it, here’s a strip from one of my favorite webcomics, XKCD.com.
About handwashing: Here’s a resource for kids
If you have young teens or younger, here’s a fun resource aimed at persuading them to wash their hands. (And if you don’t, it might tune you up to pre-teen culture):
Mitchel Musso, who plays the boy best friend on the Disney TV Show Hannah Montana, has filmed a public service announcement TV spot: “Clean Hands Are Cool Hands.”
It’s part of a campaign sponsored by the Hospital Corporation of America (HCA) and Steris Corp., which makes infection-control and surgical gear. The kid side of the site has behind-the-scenes cuteness — music, photos, video outtakes; the parent/teacher side, medical information, lesson plans, posters and stickers.
Can’t hurt. May help. Cute.

