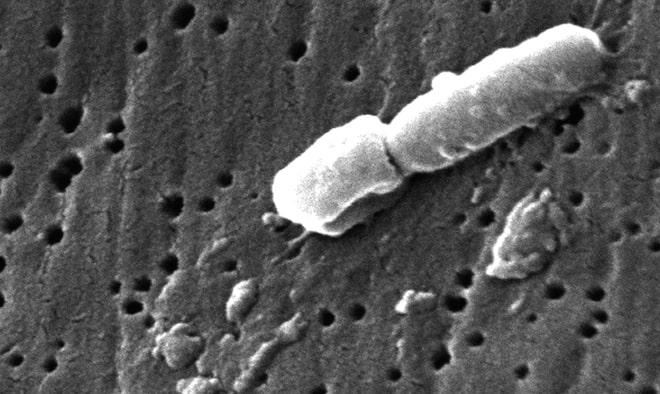
 Klebsiella, Janice Carr, CDC
Klebsiella, Janice Carr, CDC
There’s worrisome news here in the southeastern U.S., buried in a journal that is favorite reading only for superbug geeks like me. The rate at which hospitals are recognizing cases of CRE — the form of antibiotic resistance that is so serious the CDC dubbed it a “nightmare” — rose five times over between 2008 and 2012.
Within that bad news, there are two especially troubling points. First, the hospitals where this resistance factor was identified were what is called “community” hospitals, that is, not academic referral centers. That’s an important distinction, because academic medical centers tend to be where the most cutting-edge care is performed, and where the sickest people are. As a result, they are where last-resort antibiotics are used the most, and therefore where resistance is most likely to emerge. That CRE was found so widely not in academic centers, but rather in community hospitals, is a signal that it is probably moving through what medicine calls “the community,” which is to say, anywhere outside healthcare. Or, you know, everyday life.
A second concern is that the authors of the study, which is in Infection Control and Hospital Epidemiology, assume that their finding is an underestimate of the actual problem.
[Read more…]






